Hindgut Ulcers – Your Ultimate Guide
Preventing and managing hindgut ulcers is becoming an all-too-common scenario. What was once thought to be fiction has rapidly become more of a fact. Particularly as research into this area of digestion has evolved. With a positive diagnosis, it’s easy to feel as if your world has come crashing down. However, with the help of this ultimate guide, find out how to manage this problem and get your horse back to feeling healthy and happy.
When we talk about the horse’s hindgut, we’re referring to the digestive area from the cecum to the rectum. The primary function of the hindgut is to digest fibre and convert it into useable energy from volatile fatty acids. High levels of this fermentative microbial digestion take place in the caecum by microorganisms, yeast, and friendly bacteria. 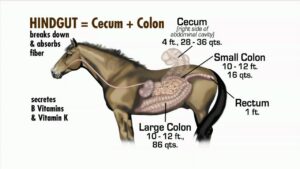
The normal acidity (PH) level in the hindgut is around 6.2. When the acidity in the hindgut is raised it lowers the pH. Lactate-producing and lactate-utilizing bacteria (bugs that cause issues) get strong in an environment with a low pH. They then start producing lactic acid rather than volatile fatty acids. This change in the microbial populations and acid profiles is what creates hindgut acidosis.
What causes this change to occur?
It’s caused by large quantities of undigested simple carbohydrates reaching the hindgut and producing lactic acid. These are usually starches and sugars found in processed grain feeds or rich pasture. This drop-in pH may reduce mucous production, leaving the mucous membranes of the hindgut vulnerable.
Furthermore, when fiber-digesting bacteria die off because of hindgut acidosis, endotoxins are released into the bloodstream. The result of this can cause issues such as laminitis.
What are Hindgut Ulcers?
- Hindgut ulcers are also known as colonic ulcers and are often referred to by vets as Right Dorsal Colitis (RDC). This is because most hindgut ulcers occur in this part of the large intestine on the right side of the horse.
- All ages and breeds of horses are susceptible. Hindgut ulcers have been reported to affect 44 – 63% of horses and are estimated to occur in 65% of sport horses. These types of ulcers can go undiagnosed for months because horses are usually normal between acute episodes.
- When hindgut health is compromised, a horse may also have trouble absorbing important nutrients. This can result in poor coat and hoof condition, reduced immune function, and behavioural changes.
- Whilst hindgut ulcers are less common than gastric ulcers, a horse can have both at the same time.
A definitive diagnosis is difficult because a gastroscope (used to diagnose gastric ulcers) won’t reach the colon.

However, one definitive method of diagnosis is a Transabdominal ultrasound. This type of ultrasound takes specialized equipment and skill on the part of the vet. If the ultrasound shows a thickened colonic wall, hindgut ulcers are likely to be diagnosed. If you’re concerned about hindgut acidity, ask your vet to test faecal pH first.
Symptoms:
Horses affected by hindgut ulcers may experience a progression of signs such as
- decreased performance, lethargy
- weight/topline loss
- reduced appetite
- diarrhea, intermittent soft manure, or “squirty” bum where some horses have a liquid component that follows passing otherwise normal manure
- mild intermittent or recurring colic
- a rough coat
- a change in attitude, sudden girthiness
- sensitivity in the flank area
- difficulty bending, collecting and extending
- blood in the manure
- chewing wood (cribbing)
- swelling (oedema) along the central midline of the belly
Why do Horses get Hindgut Ulcers?
- Stress for horses can be either physical (i.e. training and performance) and/or emotional stress (i.e. separation anxiety, floating). This leaves them at a higher risk for developing both gastric and hindgut ulcers. Additionally, stress, whether physical or mental, affects the horseʼs immune system.
- Hindgut acidosis. Usually, but not always, caused by starch overload or massive doses of pure fructan and insufficient forage. Horses with hindgut acidosis often have frequent low-grade colic, loose manure, and are off their feed.
- Overuse of non-steroidal anti-inflammatory drugs (NSAIDs). These should be used for no longer than 5-7 consecutive days. Overuse can lead to damage to mucosal membranes of the gut lining and interfere with blood clotting.
- Parasites including tapeworm, small strongyles, and others. These may also cause ulcers at the site where they attach to the intestinal wall.
- Disturbances to the gut microbiome. Eg excess levels of lactic acid are caused by a decrease in the pH level of the colon. This acidic environment may result in:
- Damage to the mucosal lining, resulting in compromised intestinal barrier function.
- Changes in the equine microbiome eg a proliferation of pathogenic bacteria and a decrease in the population of beneficial bacteria.
- Reduced defences against toxins in the gastrointestinal tract.
BE AWARE OF OTHER CONDITIONS that could look like RDC. These include
- Gastric ulcers
- Other causes of colic (large colon displacement and/or impaction)
- Infectious causes of diarrhea (Salmonellosis, Clostridium)
- Inflammatory bowel disease
- Cancer
Three Steps in the Prevention and Treatment of Hindgut Ulcers
Dietary management that prevents hindgut ulcers from recurring and to support the healing of the intestinal lining.
- Your vet may prescribe medications such as sucralfate or misoprostol.
- Reduce the amount of work the colon must do by limiting long fibre (hay) consumption. Replace it with short fibre eg hay cubes, pellets, or chopped hay.
- Offer small, frequent meals whenever possible to support gut health and improve nutrient absorption.
- Try feeding Psyllium. It can help lubricate and shorten the transit time for feed and roughage. It also increases water content in the intestines and fatty acid concentration in the colon and reduces inflammation.
- Feed to provide buffering to the hindgut i.e. beet pulp, soyhull husks
Minimizing stress is an important part of recovery from Right Dorsal Colitis. This can be done by:
- Reducing strenuous exercise or training
- Providing more turnout time
- Minimalising transport
By following as many of the above strategies, you can usually see a reduction in symptoms after 1-2 weeks. However, be aware that it can take two to three months for ulcers to fully heal.
Improve digestive health. Probiotics and prebiotics can be helpful.
Can Fibregenix Platinum Pro performance balancer help with hindgut ulcers?
Yes! Platinum Pro is invaluable in the management of hindgut ulcers. It includes 4 specific digestive aids. Actisaf Live yeast probiotic, purified nucleotides, MOS, and FOS prebiotics will tackle each of the points listed below. Each of these digestive aids has proven performance when it comes to gut health.
- For increasing the number of “good” bacteria and restoring gut health in horses with hindgut ulcers.
- To improve feed efficiency and support nutrient assimilation
- Supporting hindgut function and fibre fermentation
- Assisting in the combat of toxins by inhibiting their absorption from the gut
- Supporting the immune system by increasing immunoglobulin activity
Dietary Nucleotides are of particular interest. Here are 2 reasons why we’ve included them in our balancers for preventing and managing hindgut ulcers.
Dietary Nucleotides Improve Efficiency of Cell Growth and Repair
In general, DNA is synthesized through complicated de novo pathways. These pathways create fresh nucleotides from scratch rather than using existing material. However, in the presence of dietary nucleotides, the body can down-regulate DNA synthesis. And instead, it uses an enzyme named HGPRT to scavenge the intact nucleotides improving the efficiency of cell repair and conserving energy.
In addition to ongoing maintenance, cell division is critical for repairing damaged tissue, including ulcers. This is why in times of stress, dietary nucleotides have proven to be beneficial.
Dietary Nucleotides Increase Mucosal Thickness
Nucleotides optimize the natural protective mechanisms of the mucosal lining. This helps to maintain a healthy GI tract. Supplementing a horse’s diet with nucleotides increases mucosal thickness and protein levels through increased availability of genetic precursors. It also speeds up intestinal recovery after chronic diarrhea and intestinal damage.
Nucleotides play a critical role in the body in that they accelerate the cell regeneration process. Cell regeneration allows an animal to recover much quicker from the type of stress it is under (performance, illness, disease, injury, etc.).
TAKE HOME MESSAGE
Hindgut acidosis is a nutritional problem. You feed your horse – that makes it your problem!
Consider where your horse came from that would affect his digestion. Off-track racehorses, rescued horses, performance horses, or simply grain fed at any time in his/her life. All these will have a higher risk. In fact, any horse is at risk of hindgut acidosis from conditions that don’t support microbial digestion.
The signs of hindgut ulcers should always be taken seriously. If you suspect your horse might be affected by hindgut ulcers, get him examined by your vet as soon as possible.
In some cases, hindgut ulcers might be unavoidable. However, you can greatly reduce his chances of developing this debilitating condition. The bottom line is to limit NSAID use, minimize stress whenever possible and manage/feed your horse appropriately.